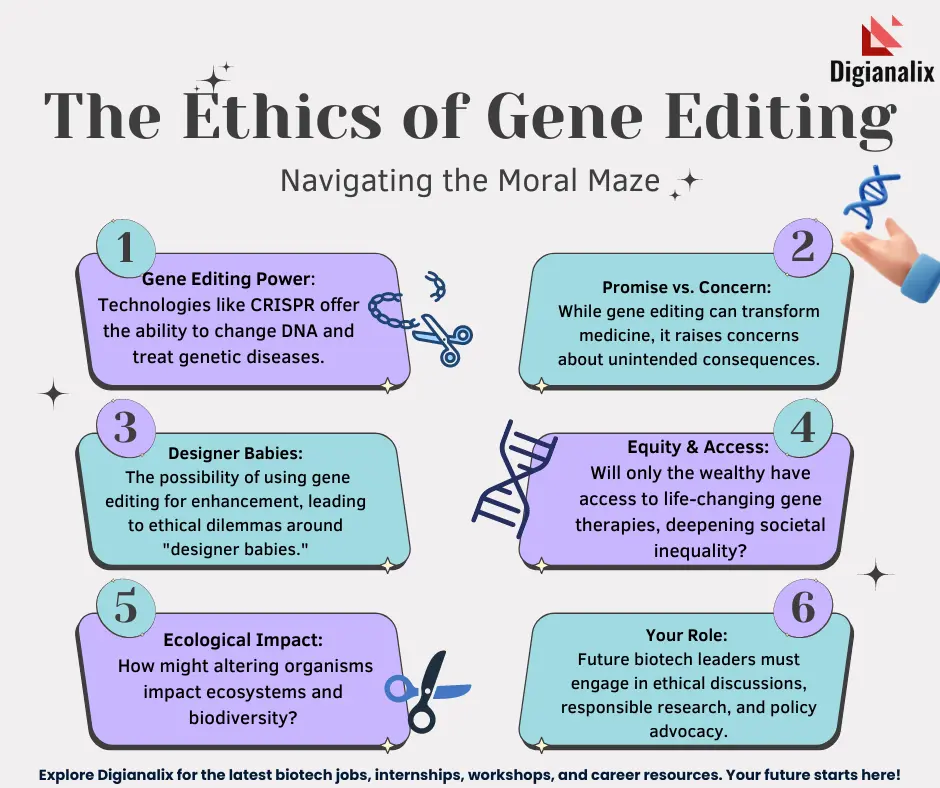
Gene editing ethics is a pivotal area of discussion in today’s scientific landscape, particularly as technologies like CRISPR make headway into the realm of genetic modification. This innovative technique holds the promise of eradicating severe genetic disorders, such as sickle cell disease, yet it simultaneously raises profound ethical implications. Do we have the moral right to alter human genetics, especially when considering health equity and the socio-economic disparities that may arise from such advancements? As experts like Neal Baer highlight the potential to cure debilitating illnesses, they also pose critical questions about who gets access to these therapies and the possible ramifications of genetic intervention. These discussions not only emphasize the need for ethical guidelines surrounding gene editing but also call for a careful examination of the impact on future generations.
The ethical considerations surrounding genetic engineering practices, particularly those utilizing techniques like CRISPR, are increasingly capturing public attention. Guided by the desire to alleviate suffering and enhance human well-being, the field of genetic modification is fraught with complex moral dilemmas. As we explore interventions for genetic conditions and the potential for enhancement, we must also weigh the consequences of these actions on our society. Public discourse must address critical issues of access to these technologies, as financial and social barriers could exacerbate existing health disparities. Ultimately, our responsibility to future generations compels us to navigate these uncharted waters with caution and deliberation.
The Promise of CRISPR Technology in Treating Sickle Cell Disease
CRISPR technology has emerged as a groundbreaking tool in the realm of genetic medicine, especially for genetic disorders like sickle cell disease. This revolutionary technique allows researchers to modify specific genes with unprecedented precision, paving the way for potential cures where traditional therapies have failed. By targeting the genes responsible for sickle cell pathophysiology, scientists can restore normal hemoglobin production, significantly improving the patients’ quality of life and longevity. The promise of CRISPR thus lies not only in correcting genetic defects but also in offering hope to countless children suffering from debilitating conditions.
However, the application of CRISPR in treating sickle cell disease raises pertinent questions about accessibility and equity. The current costs associated with gene editing treatments are staggering, with estimates around $2.2 million per patient. This astronomical price tag forces us to confront critical issues related to health equity: who can afford such treatments, and how do we ensure that advancements in genetic modification do not widen the gap between the haves and have-nots? The challenge remains to implement these transformative technologies in a manner that is fair and equitable across diverse populations.
Ethical Implications of Gene Editing in Medicine
The ethical implications of gene editing extend far beyond its clinical applications. As we harness the power of technologies like CRISPR, we must grapple with profound philosophical questions: What does it mean to alter the human experience? Should we, as a society, be allowed to modify traits that are simply variations of human diversity? These considerations were central to discussions presented by experts like Neal Baer and Rebecca Weintraub Brendel, who emphasize that the responsibilities of scientists and medical professionals are significant in navigating these uncharted waters.
Moreover, the debate over gene editing ethics also intertwines with the ideas of parental choice and societal responsibility. Should parents have the authority to choose genetic modifications for their children? This raises intricate issues of autonomy and the definition of ‘normality.’ As demonstrated in discussions during the Science Center talk, the perspectives of those who live with conditions like deafness can challenge the very notion of genetic ‘correction,’ highlighting the need to include diverse voices in conversations about genetic modification.
Health Equity: Addressing Disparities in Gene Therapy Accessibility
Health equity concerns are at the forefront of discussions about the distribution and accessibility of CRISPR-based therapies. As cutting-edge gene editing techniques are developed, they risk being available only to wealthier populations, reinforcing systemic disparities in healthcare access. The ability to afford genetic treatments like those for sickle cell disease starkly contrasts with the reality faced by many patients who do not have the financial resources to benefit from these innovations. This highlights the urgent need for policies that promote fair access to medical advancements, ensuring that everyone, regardless of socioeconomic status, can benefit from breakthroughs in genetic modification.
Addressing health equity in the context of gene therapy requires a multifaceted approach, including public health initiatives, government intervention, and collaboration with non-profit organizations. Ensuring that these life-saving treatments are accessible involves not only financial considerations but also the establishment of ethical frameworks that prioritize fairness. Engaging with communities affected by genetic disorders and inclusively designing healthcare interventions can help bridge existing gaps, ultimately fostering a more equitable health landscape.
The Risks and Benefits of Genetic Modification
While CRISPR technology heralds a new era of medical advancements, it is essential to weigh both the risks and benefits associated with genetic modification. On one hand, the potential to treat and even cure genetic disorders fundamentally transforms patient care. The prospect of eliminating diseases like sickle cell anemia through gene editing presents an optimistic future for many families. However, the application of such powerful tools carries significant risks, including unintended genetic consequences that may arise from editing complex genomes.
Furthermore, the long-term societal implications of genetic modification remain largely unknown, raising questions about the future of human evolution. For instance, if gene editing leads to enhancing certain traits, such as intelligence or physical ability, society may face ethical dilemmas regarding what constitutes ‘normal’ versus ‘enhanced’ human capabilities. The dialogue surrounding genetic modification must continuously adapt to address these evolving concerns, keeping public interest and ethical standards at the forefront of scientific endeavors.
Navigating the Regulatory Landscape of Gene Editing
The rapid advancement of CRISPR technology necessitates a thorough examination of the existing regulatory frameworks surrounding gene editing. As scientists push the boundaries of genetic modification, it is crucial that governments and regulatory bodies create comprehensive guidelines that address the myriad ethical concerns associated with germline and somatic editing. This includes setting strict protocols for research, monitoring treatment developments, and ensuring that safety standards are upheld.
Internationally, the disparate approaches to gene editing regulation further complicate the landscape. Countries like China and Russia may pursue aggressive advancements in gene technology without robust oversight, potentially leading to unethical applications of CRISPR. As the global community grapples with these issues, it is imperative to foster collaboration among nations to define ethical standards that protect human rights while promoting innovation in the field of genetic medicine.
Perspectives on Disability and Genetic Modification
The discourse surrounding genetic modification often overlooks the perspectives of individuals with disabilities. As evidenced by the discussions from the Harvard talk, voices like Carol Padden challenge conventional narratives that equate health with the absence of disability. For many, living with conditions such as deafness or albinism represents a valued aspect of human diversity rather than a pathology in need of correction. This calls for a more nuanced understanding of what it means to improve health outcomes through gene editing.
Embracing diversity in attitudes toward disability can enrich the ethical discussions surrounding gene editing. Recognizing that people with disabilities often advocate for their own needs and rights encourages a broader debate on how genetic technologies should be applied. When we include such perspectives, we can better navigate the complexities of gene editing and ensure that future innovations honor human variation rather than undermine it.
Informed Consent in Gene Therapy: A Necessity
In the context of gene editing, informed consent takes on critical importance, particularly as we consider the complexities surrounding genetic modifications. Patients and their families must understand the potential risks and benefits of treatments like those for sickle cell disease before consenting to them. Factors such as possible unintended consequences, ethical ramifications, and the long-term impact of gene interventions highlight the need for comprehensive communication and education within the healthcare system.
Furthermore, informed consent must be rooted in ethical practices that account for varying levels of health literacy among populations. As we navigate the intricate landscape of CRISPR and gene therapy, healthcare providers must ensure that patients are empowered to make knowledgeable decisions regarding their treatment options. The ongoing dialogue surrounding informed consent will be vital in building trust between medical professionals and the communities they serve.
Exploring the Future of Genetic Modification
As we venture into the future of genetic modification, the possibilities seem both exciting and daunting. Technologies like CRISPR hold the potential to revolutionize medicine by providing cures for previously untreatable genetic diseases. However, the implications of altering the human genome extend beyond health; they challenge our perceptions of identity, morality, and what it means to be human. Balancing the desire for progress with the caution warranted by our responsibilities toward ethical standards will be crucial.
The future of genetic modification necessitates ongoing dialogue among scientists, ethicists, patients, and society at large. Collaborative discussions are essential for creating a framework that governs the use of technologies like CRISPR responsibly. This holistic approach will ensure that we navigate the landscape of genetic modification thoughtfully, integrating scientific advancements with ethical considerations while fostering a society that respects and values diversity.
Community Engagement in Genetic Research
Effective community engagement is critical in the realm of genetic research and therapies, particularly as we implement groundbreaking technologies like CRISPR. Researchers and medical professionals must ensure that the communities affected by genetic diseases are both informed and involved in the discussions regarding gene editing. Engaging with these communities helps to identify social and ethical concerns, ensuring that treatment options align with patient values and needs.
Moreover, community involvement enhances the dialogue around health equity in gene therapy. By including diverse voices in the decision-making processes, we can better address the disparities that exist in access to genetic treatments. This collaborative approach not only empowers individuals but also fosters a more inclusive environment where scientific advancements can be aligned with ethical considerations and community values.
Frequently Asked Questions
What are the ethical implications of gene editing using CRISPR technology?
The ethical implications of gene editing with CRISPR technology include concerns about health equity, the potential for genetic discrimination, and the moral responsibility of modifying human traits. Many experts argue that these technologies should be approached with caution to ensure they benefit all of society and do not exacerbate existing health inequalities.
How does gene editing for sickle cell disease raise ethical questions?
Curing sickle cell disease with gene editing poses ethical questions related to the cost of treatment, access to care, and the decision-making power regarding genetic modifications. High costs, such as the approximate $2.2 million for a sickle cell cure, raise concerns about who will afford such treatments and the fairness of gene editing advancements in relation to health equity.
In what ways could genetic modification impact health equity?
Genetic modification can impact health equity by potentially widening the gap between those who can afford gene editing treatments and those who cannot. Ethical discussions around health justice emphasize the need for innovations to consider the distribution of benefits across all social strata to avoid creating inequalities in access to advanced medical technologies like CRISPR.
What role do parents play in decisions regarding genetic modification of their children?
Parents play a significant role in decisions regarding genetic modification of their children, raising ethical questions about autonomy and the rights of the child. Debates focus on whether parents should decide on genetic traits, such as selecting for health conditions or abilities, and the implications of such decisions on the child’s identity and choices in life.
What are the potential unintended consequences of gene editing?
Potential unintended consequences of gene editing include unforeseen health risks due to off-target effects and the complexity of gene interactions within the genome. Altering one gene can have cascading effects on other biological processes, as genes have evolved interactions over millions of years, which may lead to unpredicted health complications.
How does the global landscape affect the ethics of gene editing technologies?
The global landscape affects the ethics of gene editing technologies, particularly as different regulations exist in countries such as Russia or China. The lack of consistent oversight raises concerns about unethical practices, including germline editing and potential exploitation of vulnerable populations, emphasizing the need for international dialogue on ethical standards.
What is the significance of health justice in the context of CRISPR technology?
Health justice is significant in the context of CRISPR technology as it demands that innovations in gene editing consider the distribution of health benefits and burdens among different populations. Discussions highlight the importance of equity in access to these technologies, ensuring that all individuals, regardless of socioeconomic status, can benefit from advancements in medicine.
| Key Point | Details |
|---|---|
| Introduction to CRISPR | Neal Baer discusses the ethical issues surrounding CRISPR gene editing at a Harvard talk. |
| Curing Sickle Cell Anemia | CRISPR can cure sickle cell by editing somatic and germline genes, raising ethical questions about the right to change human attributes. |
| Cost and Health Equity | The cost of sickle cell treatment is around $2.2 million, raising questions about who can afford it and global health equity. |
| Ethical Decisions in Gene Editing | Debate on whether to use CRISPR for genetic conditions, like Down syndrome, or to decide desirable traits for children. |
| The Concept of ‘Human Variation’ | Carol Padden argues not all genetic traits are pathologies needing correction; diversity should be valued. |
| Oversight and Regulation | Questions about the effectiveness of regulations on gene editing globally, especially in countries with less oversight. |
| Unintended Consequences | Gene editing can have unknown effects, as exemplified by altering LDL cholesterol levels. Genes interact and evolve in complex ways. |
Summary
Gene editing ethics presents a complex landscape of considerations that merge science, morality, and societal impact. As advancements in CRISPR technology show promise in curing genetic diseases like sickle cell anemia, they simultaneously provoke profound ethical dilemmas. The crux of the debate lies in whether we have the right to alter fundamental aspects of human life, such as traits associated with disabilities. This raises critical questions regarding health equity, the cost of advanced therapies, and the responsibility of scientists, policymakers, and society at large. While gene editing offers revolutionary potential, we must proceed with caution, balancing innovation with ethical considerations to ensure fairness and justice in healthcare access.