Pediatric Cancer AI Predictions are revolutionizing the way we approach the treatment and management of childhood tumors, particularly gliomas. Leveraging advanced algorithms, this innovative technology enables clinicians to analyze a series of brain scans over time, significantly enhancing their ability to predict the risk of cancer recurrence. Traditional methods have often fallen short, leading to anxiety and frequent, unnecessary imaging for young patients. However, with the implementation of AI prediction pediatric cancer tools, healthcare professionals are now equipped to provide more accurate and timely assessments, ultimately improving patient outcomes. This pioneering approach not only reduces the burden on families but also paves the way for more personalized treatment strategies in pediatric oncology technology.
In recent advancements, the use of artificial intelligence to forecast relapse risks in childhood cancers is gaining momentum, especially for conditions like glioma. These AI-driven models utilize temporal learning to evaluate consecutive imaging results, allowing for a deeper understanding of tumor behavior over time. By assessing patients’ cancer recurrence risk, practitioners can better tailor their monitoring and therapeutic interventions. The employment of dynamic algorithms elevates the traditional cancer recurrence risk assessment paradigms, ensuring that young patients receive optimal care. As pediatric oncology evolves, technologies that integrate machine learning will continue to play a crucial role in improving survival rates and the quality of life for affected children.
Understanding AI Predictions in Pediatric Cancer Treatment
Artificial Intelligence (AI) is revolutionizing the field of pediatric oncology by providing enhanced predictive capabilities for clinicians. In recent studies, AI-based tools demonstrated superior accuracy in predicting relapse risks in pediatric cancer patients compared to traditional methods. Leveraging datasets that include longitudinal imaging, these AI models can analyze multiple brain scans over time, helping doctors make informed decisions about patient care. This marks a significant advancement in pediatric oncology technology, where the focus is on early identification of at-risk patients.
The implementation of AI prediction capabilities within pediatric cancer treatment not only streamlines the assessment process but also addresses the emotional and psychological burdens that families face. Regular follow-ups with MRIs can be extremely stressful, and accurate predictions can lead to a reduction in unnecessary imaging for low-risk patients, allowing families to focus on their child’s wellbeing rather than frequent medical visits. By utilizing AI predictions in pediatric cancer, healthcare providers can tailor interventions based on an individual’s risk profile, promoting better long-term outcomes.
Temporal Learning and Its Impact on Glioma Recurrence Prediction
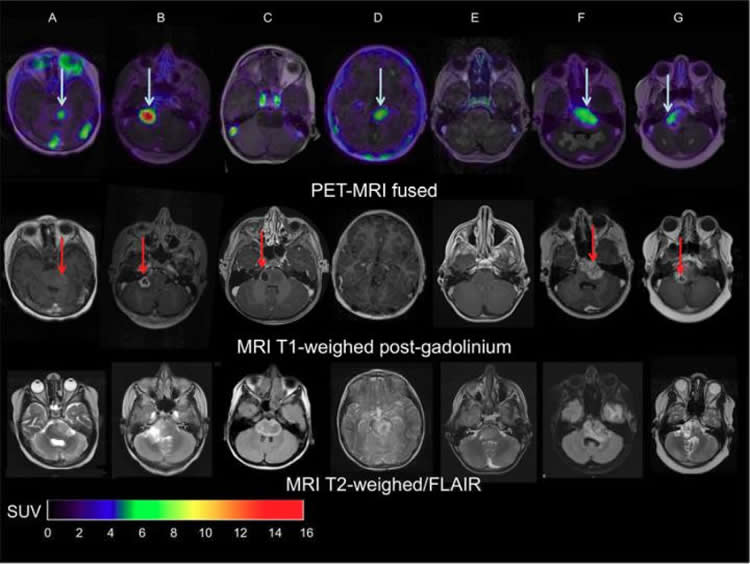
In pediatric glioma treatment, temporal learning technologies have emerged as a crucial element in accurately predicting cancer recurrence. This method trains AI algorithms to assess sequential imaging over time, rather than relying solely on isolated scans. This innovative approach allows the AI to detect minute changes in tumor progression and treatment response, linking these observations with eventual recurrence incidents. By analyzing images captured at multiple time points, researchers can achieve predictive accuracies as high as 89%, significantly surpassing traditional methods that yielded approximate accuracy rates of only 50%.
The advantages of temporal learning extend well beyond glioma management. Applications of this approach can revolutionize cancer recurrence risk assessment across various tumor types and demographic settings. As the model improves, it has the potential to inform more personalized treatment plans, significantly enhancing care protocols in pediatric oncology. Physicians can tailor follow-up imaging strategies and treatment interventions based on accurate predictions, ultimately advocating for the unique needs of each child in their care.
Advancements in Pediatric Oncology Technology
The integration of advanced AI tools in pediatric oncology marks a pivotal shift towards personalized medicine. Technologies that harness the power of machine learning and temporal data analysis are leading the charge in improving patient outcomes. The studies showcasing AI’s prominence in predicting pediatric cancer relapse bring forth a new era where treatment protocols can be informed by data-driven insights. As more clinically relevant AI applications emerge, they hold the potential to streamline pediatric oncology technologies, making early detection of relapse more efficient and effective.
Moreover, these advancements pave the way for comprehensive patient management systems that can regularly assess and predict risk factors associated with various pediatric cancers. By enabling earlier interventions and strategic treatment options, healthcare professionals can mitigate the psychological impacts on families and enhance the quality of life for young patients. Continuous investment in research and development in pediatric oncology technology is essential to harness AI’s full capabilities for the benefit of future generations.
The Future of Cancer Recurrence Risk Assessment
With the successful implementation of AI in predicting pediatric cancer recurrence, the future of cancer risk assessment appears promising. As researchers continue to refine these technologies, we anticipate even greater accuracy and reliability in identifying patients who are most at risk for relapse. This evolution will not only improve individual treatment plans but could potentially redefine entire frameworks for patient follow-up and care. Incorporating risk stratification models powered by AI will be crucial in addressing the unique challenges that arise in pediatric oncology.
Furthermore, the potential to conduct large-scale studies and clinical trials with AI insights opens pathways to broader applications within oncology. As institutions collaborate and share datasets, we can develop comprehensive models that adapt to different cancer types and patient demographics. This collaborative effort will ultimately enhance our understanding of cancer biology and improve our ability to mitigate recurrence risks, enriching the healthcare landscape in pediatric oncology.
AI and Machine Learning in Glioma Management
AI and machine learning technologies are becoming increasingly pivotal in the management of gliomas, especially in pediatric patients. Leveraging these advanced algorithms enables healthcare providers to assess treatment outcomes and predict risks associated with glioma recurrence. By analyzing a plethora of MRI scans and other imaging data over time, AI tools provide insights that allow for a more nuanced approach to patient care, helping to distinguish between types of tumors and their respective behavior.
As we further integrate AI into clinical practices, focusing on glioma management exemplifies how technology can bridge the gap between traditional medical approaches and modern diagnostic capabilities. The refinement of AI prediction algorithms, particularly in the context of pediatric patients, highlights the importance of adapting treatment plans based on the unique presentation of each case. In this way, AI not only enhances our understanding of pediatric tumors but also equips oncologists with critical tools to navigate the complex landscape of cancer treatment.
The Role of Collaborative Research in Pediatric Oncology
Collaborative research initiatives are essential in advancing the field of pediatric oncology, particularly in the context of AI-based predictions for cancer recurrence. The collective effort of institutions like Mass General Brigham, Boston Children’s Hospital, and various funding bodies forms a robust foundation for harnessing innovative technologies in clinical settings. Such partnerships enhance the sharing of knowledge and resources, crucial for developing comprehensive models that inform patient care and treatment protocols.
Moreover, through collaborative research, scientists can access larger datasets, improving model training for AI systems. As more hospitals and research institutions join forces, we can expect to see significant advancements in predicting pediatric cancer outcomes and developing more effective therapeutic strategies. By fostering collaboration, we ensure a future where pediatric oncology not only embraces the latest technologies but also prioritizes the health and wellbeing of young patients.
AI Predictions: The Key to Personalized Pediatric Cancer Care
The introduction of AI predictions into pediatric cancer care has the potential to revolutionize personalized therapy approaches. By utilizing machine learning algorithms, medical professionals can tailor treatment plans to individual patients based on their unique risk factors for cancer recurrence. This personalized approach ensures that children receive interventions specifically designed for their needs, possibly improving survival rates and reducing unnecessary therapy burden.
Personalized care through AI predictions can also empower families by providing them with clearer expectations regarding treatment outcomes. With accurate insights into a child’s condition and potential recurrence risks, parents can make more informed decisions about their child’s treatment journey. This shift towards individualized care not only enhances the therapeutic experience but also prioritizes the emotional wellbeing of patients and their families during challenging times.
Enhancing Follow-Up Protocols with AI Insights
AI predictions are set to transform follow-up protocols for pediatric cancer patients significantly. By accurately identifying individuals at high risk for recurrence, healthcare providers can modify their surveillance strategies, reducing the frequency of imaging for low-risk patients and focusing resources where they are needed most. This shift not only alleviates the emotional strain on families but also streamlines healthcare processes, improving overall patient management.
Additionally, with AI insights guiding follow-up care, oncologists can implement proactive measures, including targeted therapies for those identified as high-risk. Utilizing predictive analytics enables a more dynamic approach to patient follow-up, allowing clinicians to intervene earlier in the case of potential relapse. The integration of AI into follow-up protocols marks a critical advancement in pediatric oncology, emphasizing not only the efficiency of care but also the commitment to enhancing patient outcomes.
The Importance of Continued Research in Pediatric Cancer AI Predictions
Ongoing research into AI predictions for pediatric cancer is imperative to refine predictive models and validate their applicability across diverse settings. As AI continues to evolve, focusing on various tumor types, including gliomas, provides significant insights into cancer biology and treatment responses. By investing in this aspect of research, we underscore the importance of evidence-based approaches in pediatric oncology, which can ultimately lead to more successful therapeutic strategies.
Furthermore, persistent research efforts enable the identification of family-centric approaches to care, leading to a deeper understanding of the psychosocial dimensions of pediatric cancer treatment. By integrating AI predictions with clinical insights, healthcare professionals can develop holistic strategies that address the physical and emotional needs of patients and their families. Continuous innovation in this field is vital for establishing more effective practices in pediatric oncology and improving the quality of life for young patients.
Frequently Asked Questions
What is the significance of AI prediction in pediatric cancer, particularly in glioma relapse prediction?
AI prediction in pediatric cancer, especially for glioma relapse, is crucial as it enhances accuracy in predicting recurrence risks. By utilizing advanced algorithms, AI tools analyze multiple brain scans over time, significantly outperforming traditional single-scan methods. This technology aims to identify high-risk patients earlier, which can help tailor treatment plans and improve outcomes.
How does temporal learning enhance AI predictions for pediatric oncology?
Temporal learning enhances AI predictions in pediatric oncology by allowing models to analyze a series of brain scans taken over time. This approach helps the algorithm detect subtle changes associated with tumor recurrence more effectively than analyzing individual scans. As a result, the AI can provide more precise assessments of cancer recurrence risk in pediatric patients.
What is cancer recurrence risk assessment in pediatric patients, and how does AI contribute to this process?
Cancer recurrence risk assessment in pediatric patients involves evaluating the likelihood of a tumor returning after treatment. AI contributes to this process by analyzing data from multiple MR scans using temporal learning, which improves the predictive accuracy for recurrence. This results in better-informed decisions regarding follow-up care and potential interventions.
How effective is the AI tool in predicting glioma relapse compared to traditional methods?
The AI tool is significantly more effective in predicting glioma relapse than traditional methods. Studies have shown that it achieves prediction accuracies between 75-89%, whereas traditional approaches using single images only reach about 50% accuracy. This advancement offers hope for improved management of pediatric glioma patients.
What role does pediatric oncology technology play in the future of cancer treatment?
Pediatric oncology technology plays a pivotal role in the future of cancer treatment by integrating AI and advanced imaging techniques. This technology allows for better monitoring of tumor progression and tailored treatments based on individual risk assessments. As AI predicts outcomes more reliably, it can lead to less aggressive follow-up protocols for low-risk patients and more targeted therapies for those at higher risk, ultimately improving pediatric cancer care.
| Key Point | Details |
|---|---|
| AI Tool for Pediatric Cancer | An AI tool outperforms traditional methods in predicting relapse risk in pediatric cancer patients. |
| Significance of Findings | The AI’s greater accuracy in predicting relapse provides hope for improved care in pediatric glioma patients. |
| Temporal Learning Technique | This method analyzes multiple scans over time, enhancing prediction accuracy of cancer recurrence. |
| Study Details | Involved 4,000 MR scans from 715 pediatric patients, highlighting collaboration among prominent research institutions. |
| Training Model Accuracy | The model predicts recurrence with 75-89% accuracy, a substantial improvement over single scan predictions. |
| Future Prospects | Further validation and clinical trials are needed to assess the AI’s impact on patient care. |
Summary
Pediatric Cancer AI Predictions show considerable promise in improving treatment outcomes for young patients suffering from gliomas. The innovative AI tool developed by researchers accurately forecasts the risk of cancer recurrence, which is crucial for timely and effective interventions. As traditional methods have proven insufficient in predicting relapse, this AI-powered approach, particularly its temporal learning technique, stands to transform pediatric cancer monitoring and treatment. Further research and clinical validation will be vital in ensuring these predictions translate into enhanced patient care.